Around a third of the UK female population are thought to be going through the menopause, but many report feeling isolated and unsupported by their doctors. Can medical cannabis help manage symptoms?
“Hot sweats? It was more like a nuclear reaction,” says Lauren, a 48-year-old former mental health nurse.
“It’s awful when you’re thrown into that, you feel low and weak, it’s as though your life force is ebbing away.”
Lauren was plunged into the menopause suddenly after a hysterectomy at the age of 38.
“I literally came out of surgery, they took me up to the ward and 10 minutes later I felt as if I had an infection in my body, I was burning up,” she says.
“A doctor came over and said ‘you can’t be experiencing any symptoms yet, you’ve only just had the operation’. He just disregarded how I was feeling.”


Lauren
Working on a mental health ward for three decades, Lauren saw first hand how women were dismissed as having mental health issues, despite presenting with clear menopausal symptoms.
“We had patients on the ward aged 50 and above, experiencing suicidal thoughts, having made suicide attempts, all which [can be] linked to a chronic lack of oestrogen in the body,” she explains.
“But that was seen as a mental disorder rather than considering that it could be because they’re going into the menopause or perimenopause.”
In her own health journey, she continued to feel unsupported by clinicians and stigmatised by others who failed to understand the extent of her symptoms.
“There was a lack of understanding of not just the physical but the psychological and the emotional aspect of it. Your hormones are depleting, it’s going to affect the way you think and feel about yourself and the world,” says Lauren.
“Even at work, in the NHS, the menopause procedure from HR was to give me a fan to put on my desk. How patronising and condescending is that?”
The impact of menopause
According to the British Menopause Society (BMS), menopausal symptoms affect more than 75 per cent of women and over 25 per cent describe severe symptoms. These last an average of seven years, with one in three women experiencing symptoms beyond this.
While hot sweats are commonly linked to the menopause, many people are unaware of other symptoms, which include low mood, anxiety, depression, insomnia, low libido, poor memory and brain fog. These, amongst others, can be debilitating and have a huge impact on a woman’s daily life. And the lack of awareness and understanding mean sometimes women themselves may not realise why they are experiencing them.
Perimenopause or ‘menopause transition’ can begin years before the final menstrual period and may last for four to eight years.
Women experiencing perimenopause in particular, are less likely to be aware of what’s happening to them as the emotional symptoms can begin before any physical changes to the body, according to Dr Dani Gordon, a medical cannabis prescriber who specialises in women’s health.
“Women will come to me saying, ‘I feel like an alien is taking over my brain. I don’t know what’s wrong with me. I’m tearful all the time, or on edge and I just can’t seem to get my emotions under control’,” she says.
“These emotional dysregulation symptoms can come before the night sweats and before the periods start to get irregular, so you could still have a pretty regular cycle and still be entering into the beginnings of that transition.”
Symptoms can be so debilitating that a survey of almost 4,000 women, published in October by not-for-profit Newson Health Research and Education, highlighted that 99 per cent felt their perimenopausal or menopausal symptoms led to a negative impact on their careers.
In a BMS National Survey in 2016, 47 per cent of those who needed to take a day off indicated that they would not tell their employer the real reason behind their absence.
Despite this, menopause and perimenopause symptoms are poorly understood in the modern healthcare system. A documentary hosted by Davina McCall earlier this year started a viral conversation, the fact that it hit a nerve highlighting just how many women feel unsupported by their GPs who are often a first port-of-call for those experiencing symptoms.
Lack of understanding
According to Dr Gordon – who has heard first hand from patients and her own peers – women are frequently told to “manage their stress better”, “lose some weight” or “do more exercise” when seeking medical treatment for menopause symptoms.
“There’s so many reasons why [symptoms] may be poorly treated,” she explains.
“One of them is cultural and the fact that we don’t talk about menopause. Our culture is based on this obsession with youth and women after a certain age don’t want to talk about the transitions that they are experiencing, even though they’re completely natural and normal and everyone goes through them.”
The other factor is the medical system itself. Earlier this year it was revealed that 41 per cent of UK universities do not have mandatory menopause education on the curriculum at their medical schools. The BMS does offer additional training courses for GPs on the menopause, but these cost time and money which many simply don’t have considering the increasing pressure they are already facing.
Rachel Mason had a hysterectomy at the age of 30 after being diagnosed with ovarian cancer. She describes trying to access support with perimenopause as “horrendous” despite receiving excellent care during her cancer treatment.
“With everything else I can’t fault the care, it has been amazing but when it comes to the menopause there’s no support there,” she says.
“I tried to move my menopause clinic appointment forward as I was in a really bad place but was told they only run it once a month – can you imagine how many women need to go to that?”
As GPs have no formal training in this area, women can wait up to a year for a diagnosis, according to Dr Louise Newson, a GP and renowned menopause specialist, with only around 37 percent being offered hormone replacement therapy (HRT).
Dr Gordon believes this may be down to GPs not feeling confident in the prescribing of this treatment.

Dr Dani Gordon is a world-leading expert in medical cannabis and women’s health
She explains: “Many GPs, it seems, are not confident in the differences between body identical HRT and more traditional progestin containing HRT.
“After speaking with patients who had tried to have these conversations with their GP about wanting to try body identicals or about the specific non-drug approaches they can take for different symptoms, or about the latest research into what supplements may or may not be helpful.”
The role of cannabinoids
Dr Gordon has successfully treated many women experiencing menopausal symptoms with cannabinoids and is in the process of opening her own private integrative medicine clinic, Resilience Medicine in the UK.
“When women are going into the perimenopause phase, their ability to regulate stress usually gets worse, because the hormones are more difficult to balance, and when you throw extra stress hormones into the mix it makes the imbalances worse in the female hormones as well,” she says.
“Women are told, ‘oh just learn how to manage your stress better’, but if your hormones are raging all over the place and you have high cortisol, the stress hormone, it’s really hard to manage your stress because physiologically you’re going to be on edge, irritable, anxious, tired but wired. What cannabinoids can do is give people a tool to help get those symptoms under control.”
While menopause isn’t currently a primary indication for the prescription of cannabis-based medicines in the UK, the symptoms such as anxiety and sleep components can respond well to the treatment.
“Even if someone can’t take HRT they can still usually take cannabinoids to help with symptoms,” continues Dr Gordon.
“We have cannabinoid receptors in our womb, in our uterus, throughout our female reproductive tract, and also in the brain area, the hypothalamus that deals with the stress response. This is called the HPA axis and it also controls what’s called the HPO axis which is how the brain talks to the ovaries.
“When we introduce a high-CBD during the day and then a little bit of THC to help people sleep at night, the perimenopausal symptom clusters respond well to this in the majority of cases, because CBD can help reduce the stress response.”
Several overseas studies suggest increasing numbers of women are turning to cannabis to help manage their symptoms. A study from the University of Alberta in Canada found that one in every three women near the menopause transition uses cannabis for symptom management. Likewise, the North American Menopause Society reported earlier this year that out of over 200 women in California, who participated in the Midlife Women Veterans Health Survey, around 27 per cent reported having used or were currently using cannabis.
Lauren had been taking a high dose of HRT for around a decade when she became unwell and doctors halted the medication, fearing she was having a stroke. After being prescribed medical cannabis for primary progressive multiple sclerosis (MS) – which she was diagnosed with last year – she found it was actually helping her menopause symptoms too.
“MS is bad but some of the symptoms from the menopause were actually 20 times worse,” she says.
“Medical cannabis has given me a new lease of life. I take it in the morning and it gives me the energy to get out of the house and go to the gym.
“In the evening, if I’m having problems sleeping or with hot sweats, I take an indica strain and that just relaxes my body so I don’t feel stressed and anxious about the symptoms I am having.”

Rachel Mason is founder of Our Remedy CBD
Experiencing the benefits of cannabis also gave her the confidence to speak more openly with her GP about what she was going through. She now volunteers with PLEA (Patient-Led Engagement for Access) to help improve awareness so others can access cannabis-based medicines.
“I know how good it’s made me feel, so I’m more able to put my foot down and say ‘this is helping me, I know what I need’. Life is too short to feel unwell when there are things that you can do, you’ve got to take back the power for yourself,” she says.
“I would like to see GPs point women in a direction where they can have a discussion about medical cannabis. It might be something that they’ve never tried or they’ve been against, but it’s just about having that advocacy and giving the information to the healthcare professionals so that when they are offering choices to women they’ve got this in their toolbox.”
Tackling the stigma
Despite the fact that there are around 13 million menopausal women in the UK, it can be an isolating experience, particularly for someone going through perimenopause in their 30s as Rachel was.
“I was really scared to go through the menopause, I didn’t tell anyone because there’s such a stigma attached to it, regardless of your age, I was worried how people would react,” she admits.
“I think if I had a group of friends who were all going through it at the same time, we would talk about it and you wouldn’t feel so alone, but none of them have the same experience.
“My biggest concern was if I would still enjoy going out and socialising. I was so confused about the person I would be, but I can honestly say I don’t feel like I’ve actually changed at all.”
Rachel went on to set up her own CBD brand, focusing on women’s health. Speaking about her situation has encouraged other women in her life to open up.
“My dad’s partner was having horrendous hot flushes, she suffered for two years and didn’t know who to talk to. She was embarrassed. When I started opening up about my situation she did too and I got her started on CBD, she said they virtually stopped,” Rachel says.“Once you break through that stigma it is beneficial for everyone.”
Lauren agrees, she adds: “For me the biggest thing is the mental and emotional feelings that come with menopause, you can feel isolated, but we are 50 percent of this country, we shouldn’t feel ashamed or embarrassed. Our voices need to be heard.”
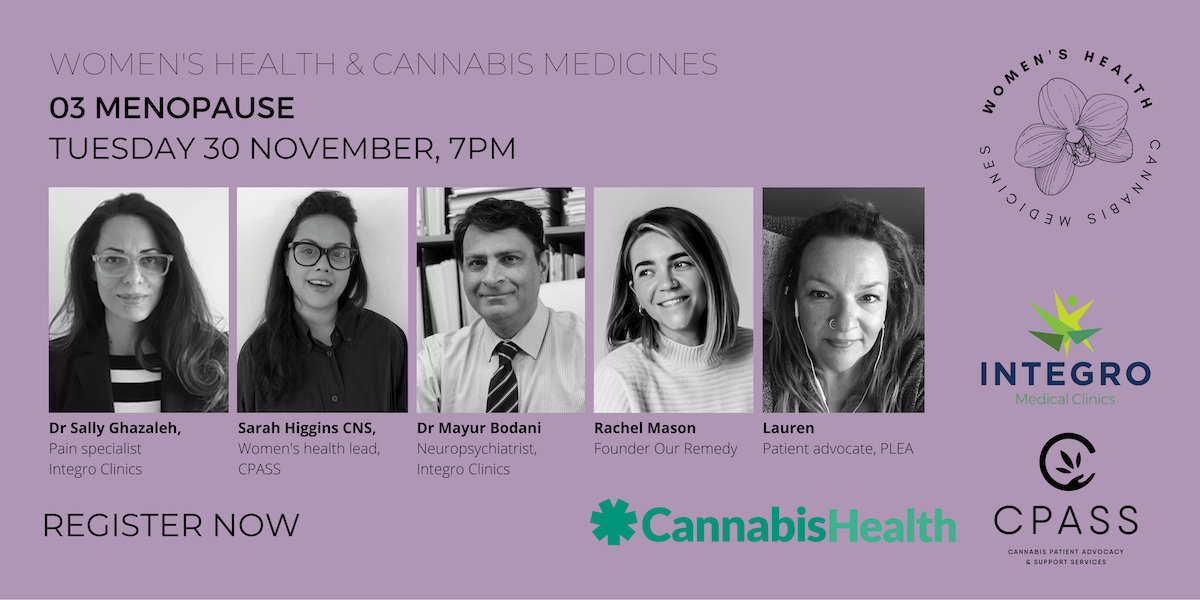
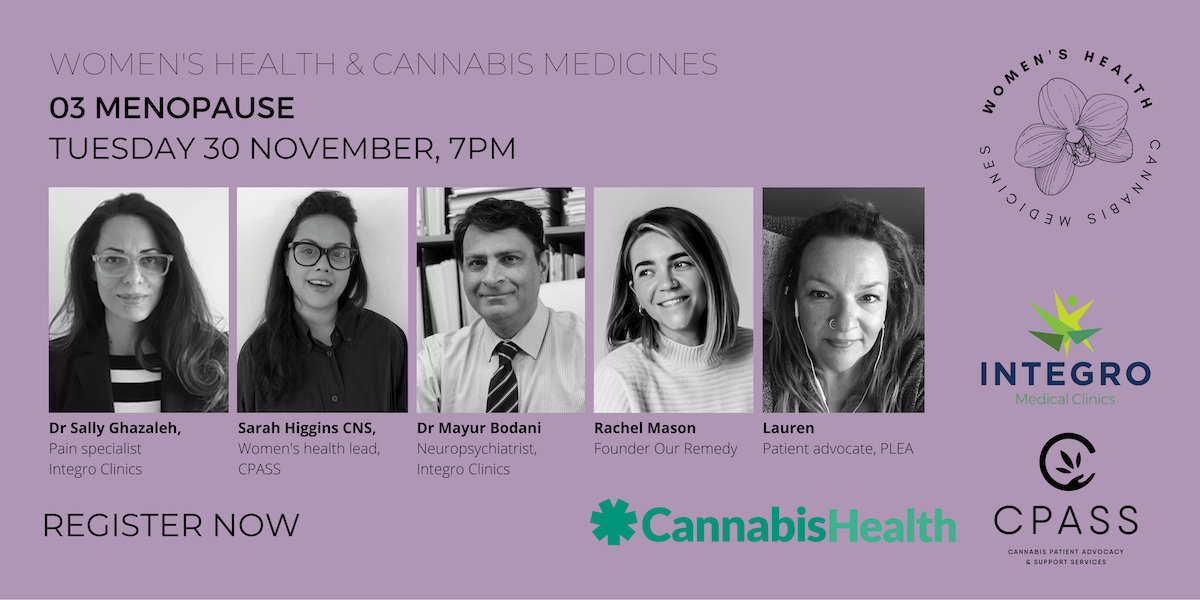
Lauren, Rachel and a panel of clinical experts will join us to discuss the experiences of women who find medical cannabis helpful in managing symptoms of menopause on Tuesday 30 November at 7pm.
Register for FREE here

 News6 months ago
News6 months ago
 News6 months ago
News6 months ago
 Science5 months ago
Science5 months ago
 Industry6 months ago
Industry6 months ago
 News6 months ago
News6 months ago
 News5 months ago
News5 months ago
 Health4 months ago
Health4 months ago
 News5 months ago
News5 months ago